Total Laparoscopic Hysterectomy (TLH) has brought about a transformative change in gynecological surgery, revolutionizing traditional approaches.
This innovative minimally invasive procedure involves the use of laparoscopic instruments to delicately remove the uterus through small incisions in the abdominal region. Compared to conventional open hysterectomy methods, TLH offers numerous advantages.
In this article, we will delve into the intricacies of TLH surgery, the array of benefits it presents, the surgical procedure itself, the recovery process, possible risks, and other relevant aspects. Whether you are contemplating undergoing TLH or simply seeking knowledge about this exceptional medical advancement, you’ve certainly come to the right place.
What is TLH Surgery?
Total Laparoscopic Hysterectomy, commonly known as TLH, is a surgical procedure aimed at removing the uterus through minimally invasive techniques. Unlike conventional open surgery, TLH utilizes small incisions in the abdomen, promoting faster healing and reduced scarring. During the surgery, the surgeon skillfully detaches the uterus from surrounding tissues and extracts it from the body.
TLH surgery can be performed in two primary ways:
Laparoscopic Assisted Vaginal Hysterectomy (LAVH): In this approach, part of the procedure is completed laparoscopically, i.e., within the abdominal cavity, while the remaining steps are conducted transvaginally through a vaginal incision.
Total Laparoscopic Hysterectomy: This method involves performing the entire procedure using a laparoscope, and the surgical specimen (the uterus) is removed through the vagina.
Candidates for TLH Surgery
TLH surgery offers a highly effective option to tackle a range of gynecological conditions, making it an excellent choice for individuals dealing with the following problems:
Uterine Fibroids: These are non-cancerous growths in the uterus that can lead to pain and heavy menstrual bleeding.
Endometriosis: This condition involves the abnormal growth of the uterine lining outside the uterus, resulting in pain and potential fertility issues.
Uterine Prolapse: It refers to the downward displacement of the uterus, causing discomfort and urinary problems.
Chronic Pelvic Pain: This condition involves persistent pelvic pain that significantly impacts a woman’s quality of life.
Gynecologic Cancer: In certain cases, TLH surgery might be utilized as a treatment option for gynecologic cancer.
Advantages of TLH Surgery
1. Minimally Invasive Approach
2. Reduced Blood Loss
3. Shorter Hospital Stay and Faster Recovery
4. Lower Risk of Complications and Infection Rates
5. Preservation of Ovaries
In many cases, TLH allows for the preservation of the ovaries, maintaining hormonal balance in premenopausal women.
Other notable advantages include less post-surgery pain than with laparotomy (open surgery), fewer wound complications, potentially lower risk of Deep Vein Thrombosis (DVT) due to quicker mobilization, reduced risk of bowel or bladder dysfunction, and a shorter hospital stay.
The TLH Surgical Procedure
Before the Procedure:
During the Surgery:
TLH is typically performed under general anesthesia while the patient is asleep. A cannula, a narrow plastic tube, is inserted into a vein in the arm or hand using a needle to administer fluids and medications. A catheter is also inserted into the bladder to facilitate urine drainage. The surgical process involves the following steps:
- Incision: A small cut (about 2 cm) is made below the navel (belly button).
- Laparoscopy: The abdomen is filled with gas, and a laparoscope (optical instrument) is inserted to view the internal organs. Three more small incisions, each about 1 cm, are made on the abdomen to insert other instruments.
- Removal of Uterus: Depending on the specific case, the ovaries, and fallopian tubes may or may not be removed. In most cases, the uterus and cervix are removed through the vagina. If the uterus is too large to be removed vaginally or the vagina is narrow, a slightly larger incision is made on the abdomen for extraction.
- Wound Closure: The incisions are closed with dissolvable stitches. The entire procedure typically takes around 1 to 2 hours, with the patient spending approximately 3 to 4 hours in the operating room and recovery.
Risks and Complications
Minor Risks:
- Inflammation, Infections, and Bruising in Abdominal or Vaginal Wounds
- Hematoma (Blood Collecting in the Wound)
- Chest Infection
- Urinary Tract Infections (e.g., Cystitis) occurring in approximately 1 in 6 women
- Hernia
- Adhesion (Tissue Sticking Together)
More Serious Risks:
- Injuries to the Bladder, Ureters, Bowel, or Blood Vessels.
- Heavy Blood Loss, occasionally requiring a blood transfusion.
- Anesthetic Risks, which your doctors will discuss with you, including any medical conditions that may heighten these risks.
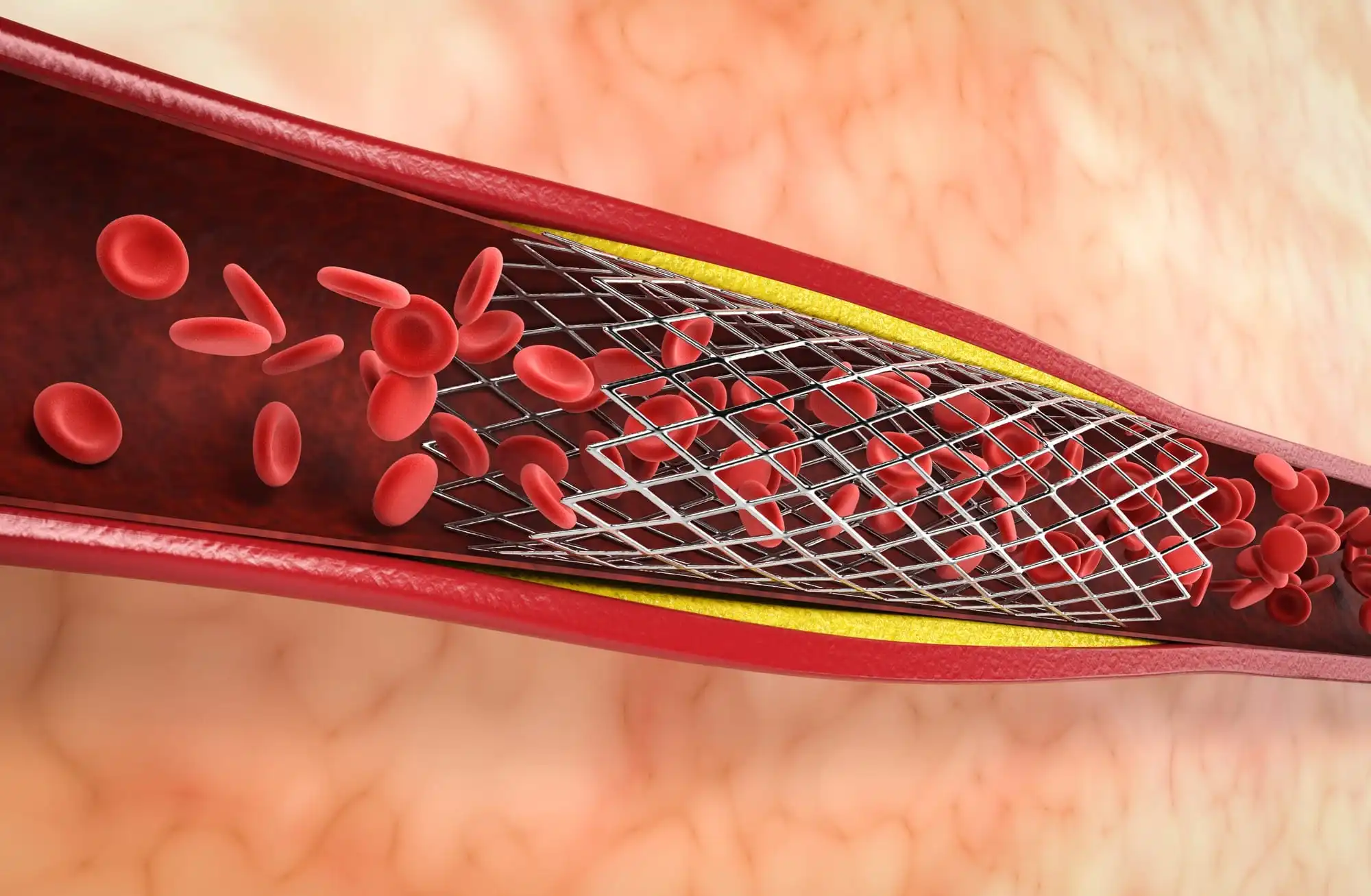
- Thromboses (Blood Clots in the Leg or Chest), which are rare after this surgery and are usually addressed with preventative treatment.
Aftercare
Following TLH surgery, patients may require a short hospital stay for monitoring and pain management. The length of the hospital stay varies based on individual circumstances but is generally shorter than with traditional open surgery.
Patients will receive pain medication to manage any discomfort during the initial days after surgery. Most patients can resume light activities within a few days to a week after TLH surgery, although strenuous activities and heavy lifting should be avoided for several weeks to ensure proper healing.
Regular follow-up appointments with the surgeon are essential to monitor the healing process and address any concerns that may arise. Using a Personal Health Record (PHR) app like Health-e can be highly useful in facilitating follow-up care with a surgeon after TLH surgery. Such apps allow patients to conveniently track and manage their medical information, making the postoperative follow-up process more efficient and effective.
Final Thoughts
TLH surgery represents a significant leap forward in the field of gynecological surgery, offering numerous advantages over traditional open procedures. With its minimally invasive approach and faster recovery times, TLH has become a preferred option for treating various uterine conditions.
If you are experiencing gynecological issues that may require surgical intervention, consult with your healthcare provider to determine if TLH surgery is a suitable option for you.