Black fungus, scientifically known as mucormycosis, has become a growing concern, especially for people recovering from COVID-19. This rare fungal infection, can be a severe and even deadly disease if not diagnosed and treated early.
Surprisingly, studies have shown that more than 5 crore Indians are affected by serious fungal diseases, and 10% of them are dealing with the potentially dangerous black fungus infection. News from around the world has been full of alarming reports about this hidden infection, leaving many of us confused and worried.
In this article, our aim is to help you understand black fungus (Mucormycosis). We’ll explore its different types, uncover the causes, examine the symptoms, discuss the available treatment options, and provide valuable insights into this important health concern.
What is Black Fungus or Mucormycosis?
Mucormycosis, commonly known as Black Fungus, is a rare fungal infection caused by a group of fungi known as ‘mucormycetes.’ These fungi are typically found in the environment, particularly in places like compost, soil, leaves, animal dung, and decaying organic matter. Infections occur when these fungi enter the body through various means, such as open wounds in the skin or inhalation.
Once inside the body, these fungi have the potential to affect different organs, including the skin, brain, lungs, and sinuses. The severity and type of infection depend on the site of entry and the patient’s overall health.
Types of Black Fungus or Mucormycosis
Mucormycosis can be classified into various types such as:
- Pulmonary Mucormycosis (Lung): This type is most prevalent among cancer patients and those who have undergone stem cell or organ transplants.
- Rhinocerebral Mucormycosis (Sinus and Brain): Common in individuals with uncontrolled diabetes and those who have received kidney transplants, this type begins in the sinuses and can spread to the brain.
- Cutaneous Mucormycosis (Skin): Typically occurring in people with no weakened immune systems, this form arises when fungi enter the body through damaged skin resulting from surgery, severe burns, or injuries.
- Gastrointestinal Mucormycosis: Primarily affecting young children, particularly those with low birth weight and premature infants under one month old, this type can develop post-surgery or due to medication that compromises the body’s ability to combat illness.
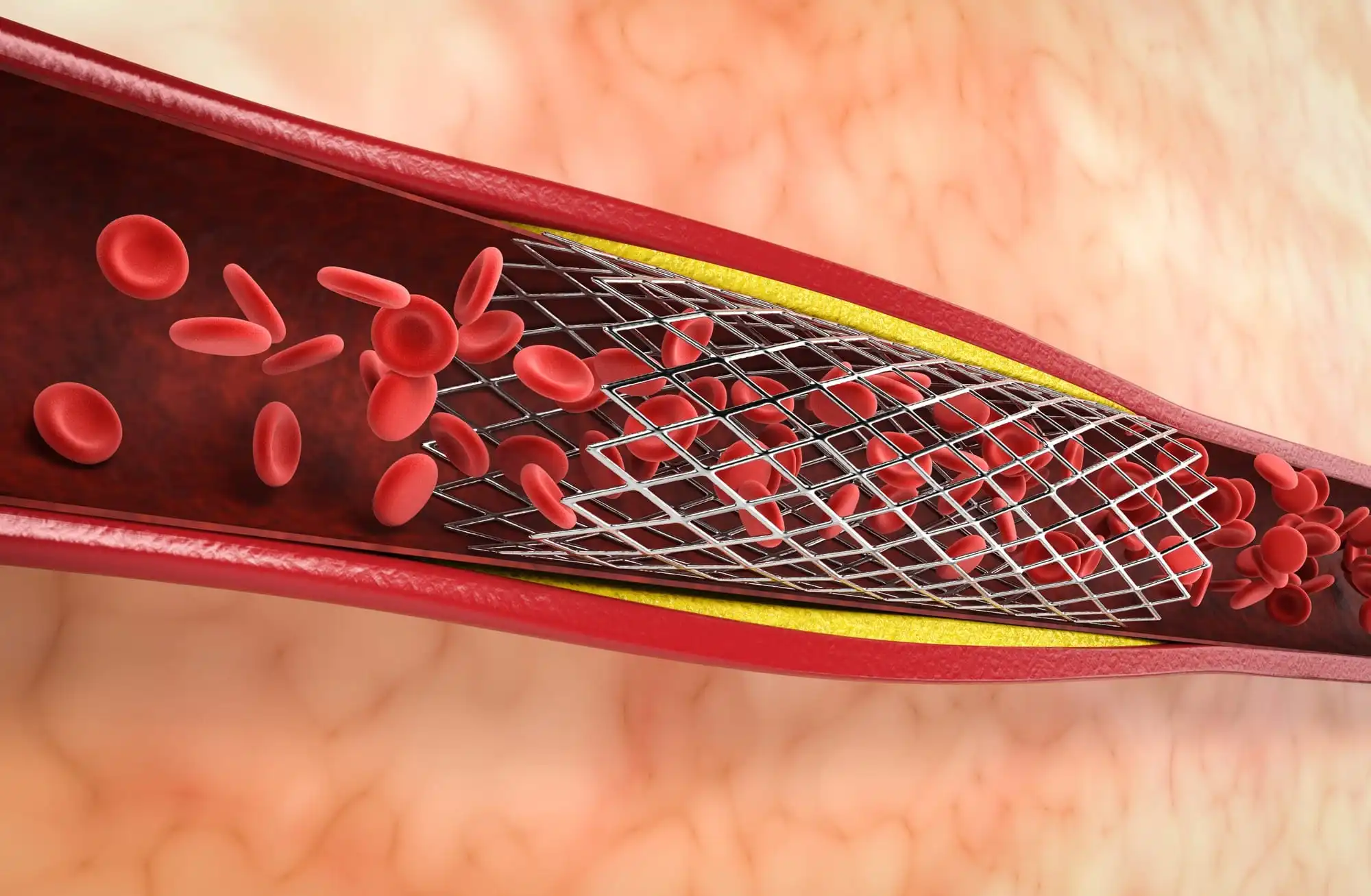
- Disseminated Mucormycosis: This widespread infection, often targeting the brain and central nervous system, spreads through the bloodstream, affecting multiple body parts and organs, including the heart, spleen, and skin.
Causes of Black Fungus or Mucormycosis
Mucormycosis can result from inhaling fungal spores from the environment, leading to lung, brain, or sinus infections. Additionally, the fungus can enter the body through damaged skin due to injuries, surgeries, or other skin trauma. While microscopic fungal spores are common, they typically do not harm individuals with healthy immune systems. However, for those with weakened immune systems, inhaling mucormycete fungi spores can trigger infections that may spread to other parts of the body.
Common fungi species responsible for this infection include Rhizomucor, Mucor, Rhizopus, Cunninghamella bertholletiae, Saksenaea, Syncephalastrum, Apophysomyces, and Absidia.
Symptoms of Black Fungus or Mucormycosis
The symptoms of mucormycosis can vary depending on the affected area of the body and may include the following:
- Fever
- Cough
- Chest pain
- Shortness of breath
- Swelling on one side of the face
- Headache
- Sinus congestion
- Black lesions on the bridge of the nose or inside the mouth
- Abdominal pain
- Nausea and vomiting
- Gastrointestinal bleeding
- Blood in the stool
- Diarrhea
- Skin infections may appear as blisters, redness, swelling, or blackened skin, accompanied by warmth or pain.
In more serious situations, if the infection spreads through the bloodstream, it can impact different parts of the body such as the spleen and the heart. At this point, it can cause alterations in mental state or even result in a coma, potentially leading to death.
Now, let’s explore specific symptoms associated with each type of Mucormycosis
1. Lung Mucormycosis (Pulmonary)
- Trouble breathing
- Chest pain
- High fever (over 100°F)
- Coughing up bloody or dark fluids
- A persistent cough
- Swelling on one side of your face
2. Sinus and Brain Mucormycosis (Rhinocerebral)
- Fever
- Headache
- Stuffy or congested nose
- Swelling on one side of your face
- Black spots in your mouth or on your nasal bridge
3. Skin Mucormycosis (Cutaneous)
- Pain in the affected area
- Small, fluid-filled blisters on your skin
- Skin sores or infections in certain areas of your face
- Darkening of the infected skin
- Warmth, redness, and swelling around the infection
4. Gastrointestinal Mucormycosis
- Feeling nauseous and vomiting
- Pain in your abdomen or stomach
- Gastrointestinal bleeding
5. Disseminated Mucormycosis
- Swollen eyelids
- Weakness in the muscles around your eyelids
Who is at Risk of Black Fungus?
- Patients prescribed steroids as part of their COVID-19 treatment
- Individuals who have undergone organ transplants or stem cell transplants
- Those with chronic illnesses
- People with uncontrolled diabetes
- Infants with low birth weight
- Premature infants
- Those on medications that weaken the immune system
Diagnosis of Black Fungus
If you’re worried about mucormycosis, your doctor will conduct a physical test and ask about your health history. Let them know if you’ve been around bad food or places with mold. If they think you have a lung or sinus infection, they might take some fluid from your nose or throat for testing. Sometimes they’ll need a small piece of infected tissue for tests, too. They might also use CT or MRI scans to see if the infection has spread to your brain or other parts.
In times like these, using PHR Apps like Health-e can be super helpful. It helps you keep your medical info organized, so you don’t have to carry papers around. Plus, your doc can treat you better if they can see your whole health history. So, go ahead and download Health-e today and take charge of your health.
Treatment of Black Fungus
If diagnosed with mucormycosis, timely initiation of antifungal medications is essential to combat the infection. Commonly prescribed medications include Amphotericin B, Isavuconazole, and Posaconazole. These medicines basically stop the fungus from growing, kill it off, and manage the infection.
Depending on how bad it is, you might have to take these meds through a drip or just swallow them. Surgical intervention might be necessary in severe cases to remove infected or dead tissue and prevent the further spread of the fungus. Although such procedures may lead to disfigurement, they are crucial for treating this life-threatening infection.
Prevention of Black Fungus
- Avoid high-dust environments, such as construction sites, or wear N95 masks for protection.
- Steer clear of contaminated water, especially in flood-prone areas and water-damaged buildings.
- If you have a weakened immune system, refrain from activities involving dust or soil. If necessary, protect your skin with appropriate clothing, and immediately wash any cuts or scrapes with soap and water.
Closing Thoughts
If you’ve been diagnosed with mucormycosis, it’s really important to stick to the treatment plan your doctor gave you. If you ever notice any side effects or have worries, don’t hesitate to talk to your healthcare provider about them. And if you ever find it hard to breathe, seek medical help right away.
By learning about the risks, symptoms, and how to prevent black fungus, we can all do our part to stay healthy and safe, especially during these tough times.
Frequently Asked Questions (FAQs):
1. Is Black Fungus Communicable?
Mucormycosis is a non-contagious disease that cannot transmit by direct or indirect contact between people or between people and animals.
2. How is Black Fungus Caused?
Black fungus infection, also known as mucormycosis, is caused by mucormycetes, a type of fungus. The fungus is present in the soil, rotting wood, a pile of compost, and leaves. The infection can occur when spores of the fungus are inhaled or come in contact with the skin, the risk of which is higher in people with weakened immune systems, uncontrolled diabetes, and those who have been on prolonged use of steroids.
3. Can Black Fungus Be Cured?
4. How to Detect Black Fungus?
AIIMS has issued guidelines for detecting and caring for black fungus or mucormycosis cases. Here are some signs and symptoms that can help detect black fungus infection:
- Abnormal black discharge or crust or blood from the nose.
- Nasal blockage, headache, or eye pain, swelling around the eyes, double vision, redness of the eye, loss of vision, difficulty in closing the eye, inability to open the eye, prominence of the eye.
- Facial numbness or tingling sensation.
- Difficulty in chewing or opening the mouth.
- Regular self-examination: Full face examination in daylight, for facial swelling (especially nose, cheek, around the eye) or black discoloration, hardening, and pain on touch.
Loosening of teeth.
If you experience any of these symptoms, it is advisable to consult a doctor immediately. The diagnosis of black fungus infection involves a test that measures galactomannan, a molecule found in the cell wall of Aspergillus fungi.